Scientists know there is a link between obesity and some cancers. A study in mice and people suggests why a high-fat diet increased the number of Desulfovibrio bacteria in the guts of mice, suppressing their immune systems and accelerating tumor growth. Studies of how to show that correlation is causation.
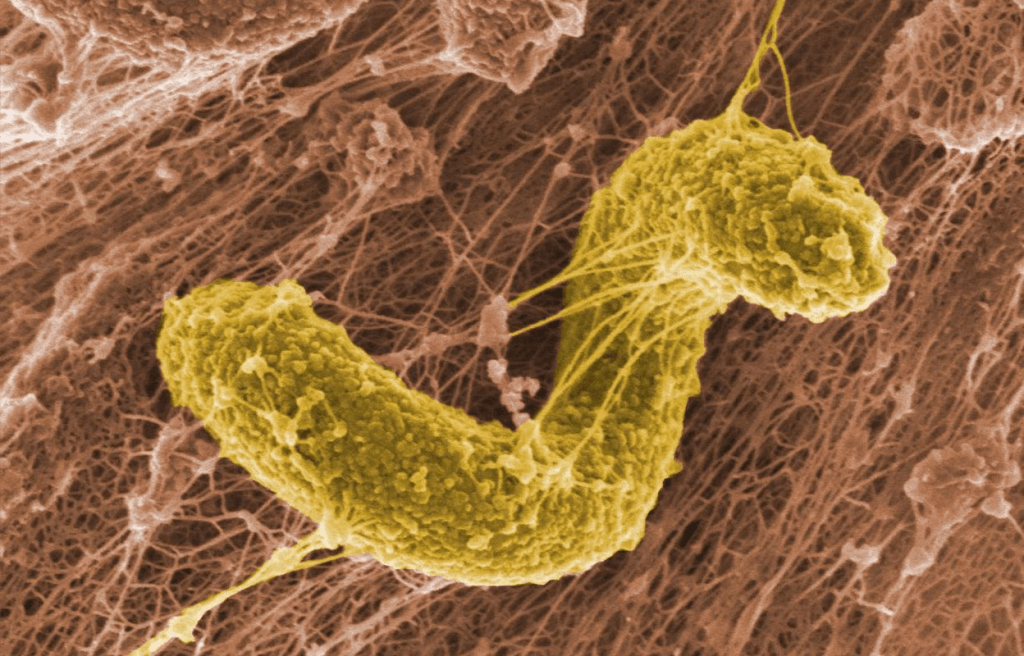
A Desulfovibrio bacterium. This group of gut bacteria has been linked to a suppressed immune system, which can allow breast-cancer tumors to flourish. Credit: PNWL/Alamy
Judah Pearl’s treatise in The Book of Why has laid to rest the idea that the notion of causality should be avoided in science. Here’s an example from scientists in China about how a high fat diet causes cancer.
Besides making you old by inducing cellular senescence, keto diets increase your probability of cancer. Let’s look at how keto diets cause cancer. Published in PNAS, researchers sampled tissue and fecal from 61 people with breast cancer at the SunYat-Sen Memorial Hospital in China, before the participants started treatment. Women whose BMI exceeded 24, the authors’ threshold for obesity classification, had higher levels of bacteria in the Desulfovibrio genus than did those whose BMI was lower than 24.
Next, the scientists in China used mice to further explore this link. Mice that are fed a high-fat diet often serve as a proxy for human obesity in animal studies. The team found that mice consuming a high-fat diet had more Desulfovibrio bacteria and had elevated levels of a type of cell that suppresses the immune system, myeloid-derived suppressor cells (MDSCs), which originate in the bone marrow. This suggested to the researchers that higher numbers of Desulfovibrio bacteria, a type of dysbiosis, and a suppressed immune system were linked.
The next clue. The mice fed a high-fat-diet mice also had higher levels of the amino acid leucine circulating in their blood than did mice fed a normal diet. Knowing that leucine can be made by particular types of gut bacteria, the team treated the mice with antibiotics that killed Desulfovibrio. Treatment caused both MDSC and leucine levels to return to normal.
With knowledge gained from the mice studies, the researchers returned to the blood samples that they had taken from the people with breast cancer. Correlating with the mice studies, those with a BMI of more than 24 had higher levels of leucine, more immunosuppressive MDSCs and survived fewer years post-treatment than those with a lower BMI. This means Desulfovibrio bacteria benefited from a high-fat diet and made excess leucine. This caused a spike in the numbers of MDSCs, which suppress the immune system and allow tumors to grow.
Their findings reveal that the “diet-gut–bone marrow–tumor” axis is involved in high fat diet-mediated cancer progression and opens a broad avenue for anticancer prevention strategies by targeting the aberrant metabolism of the gut microbiota through dietary modification. You are what you eat, and so are the microbial co-inhabitants of your body. It’s time for everyone to be “Thinking and Eating for Two.”
